*Note: the above image is representative of a pediatric open heart surgery, but was not taken during the following procedure.
Twenty-one floors in the sky is not enough to escape the chaotic cacophony of Mumbai’s crowded streets. Yet there is one place you can go and find concentrated quiet: the operating theater.
The Theater, Oh, the Theater
Indeed, surgery is an elaborate dance, a coordinated performance. The cardiopulmonary bypass* machine hums, the surgical scissors snip, the brows furrow. The surgeon glances.
9:30AM. July 23, 2018, or, in India, 23/07/2018 at 0930.
“I heard that you work in cardiology, right?” He asks me, swiftly and delicately suctioning blood from the cavity around the heart, revealing pink and gleaming. Oh, and moving, almost like a small being was trapped inside it, struggling to push its way out of a sack, rhythmically caught in the dance of the escape. Coordinated, and beautiful (at least, I think so). The bare human heart.
*Medical definitions are bolded and italicized, and located at the bottom of this page.
“I’m going to enter through the PA.” Snip, snip. Whirr, whirr. Tick tock. Time hovers, like a storm cloud filled with impending wetness, forcing you to race. The surgeon races against the impending knowns: the long bypass times, cross clamp times, and ischemic times that correlate with these slightly less knowns: the risks that aren’t so sure. And the surgeon balances speed with dexterity with habitual, evidence-based, data-driven surgical technique: it’s all part of the process.

7 AM. The time when the induction began. Place the arterial line. Get more IVs. Intubate. The anesthesiologist’s work is never done, but her moment on the stage is then: the dress rehearsal, the opening scene. After, she floats in and out, somehow appearing right when she is needed, peeking over the thick, green curtain that separates her corner from the production. Now, she is backstage. She comes in for moments, but in much, she waits and watches.
“Cardioplegia.”
Beep, beep, beeeeeeep. The tiny being in the heart no longer struggles to get out. He lays still now, in his immoveable sack, and enters a deep, cold rest. The reassuring, consistent pattern of sharp green mountains rising above valleys slows and…flatline. The EKG reading is gone; the hollow, empty “zero” remains. The heart is…dead, but then it will be resurrected.
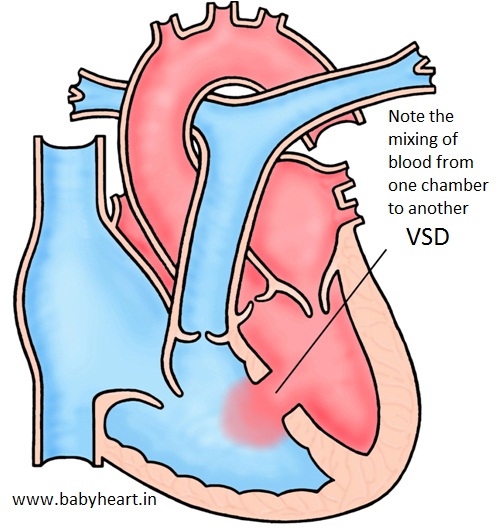
The heart is a small, 6-month old’s heart, cautiously sacrificing itself to the steady movement of the surgeon’s knife. Layer after layer. Suction. Snip snip. Slice. Repeat. I see wispy, white valves emerge, like tiny petals and feathers. “Do you see the VSD?” There it is, in all its tiny, hollow glory: how can something so small, something that is actually nothing-a mere hole-be so powerful? To dictate a child’s life in such a profound way? To require the many years of study and artful training, and a team of 8, working as a machine: steady, standardized, programmed. But, then the solution to the hole-y nothingness. The surgeons snips again: this time an oval, cut out of a piece of white material, slowly stitched in, like a patch of a quilt. But this is no patch of a quilt. This is the patch of the heart. Stitch, stitch. The hole becomes naught.
The surgeon also performed a muscle resection for some mild pulmonary stenosis, and began stitching up the holes he had left. When everything was in place, stitched back into its gleaming case, the process was reversed: and to death, life was given. Warmth, and movement, in a slow, staggering, uncoordinated way. You could see it in the ugly, jagged lines of the green mountains and valleys of the EKG, and in the slow heart rate number-too slow for a baby. Always harmonized, always focused, the human machine continued to turn its wheels. Critical thinking and teamwork hung in the air like the thick humidity hangs about Mumbai’s streets, and before a moment we heard, “Charging.” Hands away. Electricity applied. Shock. The defibrillator quieted. The 0 emerged, then the green mountain peaks and valleys returned to their coordinated dance, and the human machine whirred on.
Echocardiogram.
Muffled language. Confabulation (one of my favorite words). Rushed questions. Discombobulation (another one of my favorites). Josh whispered in my ear with a grin, “The echo looks like an angry face.” A hasty phone call, and a new face appeared: a mask-covered, blue scrub wearing one, full of more knowledge, competence, and opinions. A friend? A consultation. Tricuspid, tricuspid, tricuspid. No sighs, only a continuation of the human machine. The team never stops until the work is done, the heart made whole. However, the process would have to be momentarily reversed: though the heart was now, again, stitched, fixed, it would have to be unstitched. Sometimes, things get worse before they get better. “Tricuspid regurg-new, I should add,” the surgeon explained in manner-of-fact tone and gesture. He would explore it, check the valvular competency, decide what to do. Not ideal-another race against time: a longer surgery, a (probably) slower recovery, more risks. But better to deal with a new problem now than to ignore it and hope it never shows its ugly face.
Almost four hours had gone by this point, and we had to leave for another meeting. At the next private hospital, the COO told us that, while most patients paid out-of-pocket, some of the hospital’s funds were allocated towards free procedures for those who could not pay. “For example, children with heart conditions come from all over India for free pediatric cardiac surgeries. Other centers do them, too.” We smiled. “We actually saw one this morning-a VSD patch closure-at the Asian Heart Institute. It was…amazing.” We left, full of three things:
- Full of strong, spicy tea
- Full of new thoughts about healthcare challenges and opportunities in India
- Full of heart–for, while my healthy & complete heart beats, many babies are born with incomplete hearts that struggle to beat. But, despite the lack of access to quality, affordable healthcare that many Indians face, at least many babies’ hearts will beat anew thanks to the skillful, compassionate care of some of Mumbai’s finest hospitals.

Definitions: for those who aren’t fond of blood and seeing human hearts (or, more simply, for those that don’t work in medicine):
Cardiopulmonary bypass: the external “heart and lung” machine that temporarily relieves the heart and lungs of these functions during surgery by circulating blood and its contents (oxygen, carbon dioxide, etc.) throughout the patient’s body
PA: pulmonary artery-the blood vessel that connects the right side of the heart to the lungs. This artery carries “blue,” deoxygenated blood to the lungs for re-oxygenation.
Bypass times, cross clamp times, and ischemic times: Simply put, during open-heart surgeries with the heart-lung bypass machine the surgical team keeps track of the amount of time the patient is in a certain clinical stages (for example, “bypass time” is how long their body is reliant on the cardiopulmonary bypass machine). This allows better prediction of post-operative clinical events associated with times that are longer than a certain threshold (depending on the type of surgery).
Induction: As many would say, “putting the patient under” or “to sleep” for surgery
Arterial line: A line, similar to an IV, that instead of a vein is placed into an artery, and allows for moment-by-moment accurate monitoring of blood pressure.
Intubate: Putting the breathing tube into the patient. The breathing tube is then attached to the mechanical ventilator, which “breathes for the patient” during surgeries, intensive care, and emergency situations.
Cardioplegia: A solution that temporarily stops-or paralyzes-the heart for cardiac surgery. This is later reversed.
VSD: Ventricular Septal Defect-the primary heart defect of the patient, and the reason for surgery. There are four chambers in the heart: two atria (on the top) and two ventricles (large, muscular chambers on the bottom that pump blood out of the heart). Some children are born with a hole between the two ventricles, called a VSD.
Pulmonary stenosis: Remember the pulmonary artery we discussed above? Well, sometimes there is some kind of obstruction to blood flowing smoothly through the vessel-it could be a problem with the valve, or thickened muscular tissue at some point of the vessel. Depending on the type of pulmonary stenosis, this may require various types of intervention, such as a…
…Muscle resection: If the pulmonary stenosis is caused by thickened tissue that is impeding blood flow, sometimes some of this tissue needs to be surgically removed
Echocardiogram: sometimes called an “ultrasound of the heart”
Tricuspid (valve): there are four valves in the heart, two for each side. On the right side of the heart, the tricuspid valve is the doorway between the top chamber (right atrium) of the heart and the bottom chamber (right ventricle)
Tricuspid regurg(itation): Shortened, tricuspid regurg. If a valve doesn’t close as well as it should, blood leaks backwards through the “door.” In this case, when blood goes from the right atrium into the right ventricle, it shouldn’t be able to go backwards. If there is tricuspid regurgitation, some blood leaks back into the right atrium. This may create more clinical problems, and may require surgical intervention.
